Kevin Tabb, MD (CEO & President, BILH) discusses how the system has been preparing for a second surge and is confident going into the winter now that teams have had experience with COVID-19 and time to stock up on protective gear, medical equipment, test kits, and therapeutics.
Boston Globe – November 14, 2020
‘We are stronger now than we were then’: Mass. hospitals better prepared for a second virus surge

Massachusetts hospitals are bracing for another surge in coronavirus cases, preparing to quickly add beds and ramp up treatment should the number of seriously ill patients soar again as it did last spring.
Doctors and hospital officials are concerned about the growing numbers — hospitalizations in the state have nearly quadrupled since Labor Day — but so far, they don’t expect a sudden crush of patients whorequire life-saving treatment like last March and April. Around the United States, however, the number of COVID-19 hospitalizations hit all-time highs last week, with over 69,000 reported as of Saturday, including more than 13,000 people in intensive care.
COVID case numbers are also spiking again in Massachusetts — 2,841 new cases were confirmed on Saturday, and the state has passed 10,000 deaths in total— but there are important differences from the surge in the spring, and the experience inother parts of the country.
In Massachusetts, the rate of hospitalizations is rising more slowly than the rate of new cases, and more gradually than earlier in the pandemic. The people testing positive now tend to be younger and less likely to require hospitalization and intensive care. The death rate has improved. And because doctors now know more about COVID-19 and how to treat it, patients oftenrecover more quickly and spend less time in hospital beds.
The comparison with other parts of the country is complicated, with the differences due at least in partto local restrictions and people’s behavior. Some states, like Wisconsin, North Dakota, and Wyoming, are experiencing their first major surge and haven’t flattened the upward curve of the outbreakyet. Massachusetts’ stay-at-home advisory, restrictions on gatherings, and closures of bars and indoor spaces are more stringent than in most other locales.
And Massachusetts residents appear to be better at adhering to public health recommendations to wear masks and maintain distance from others, helping to keep transmission of the virus here below the levels now seen in many other states, hospital and state officials say.
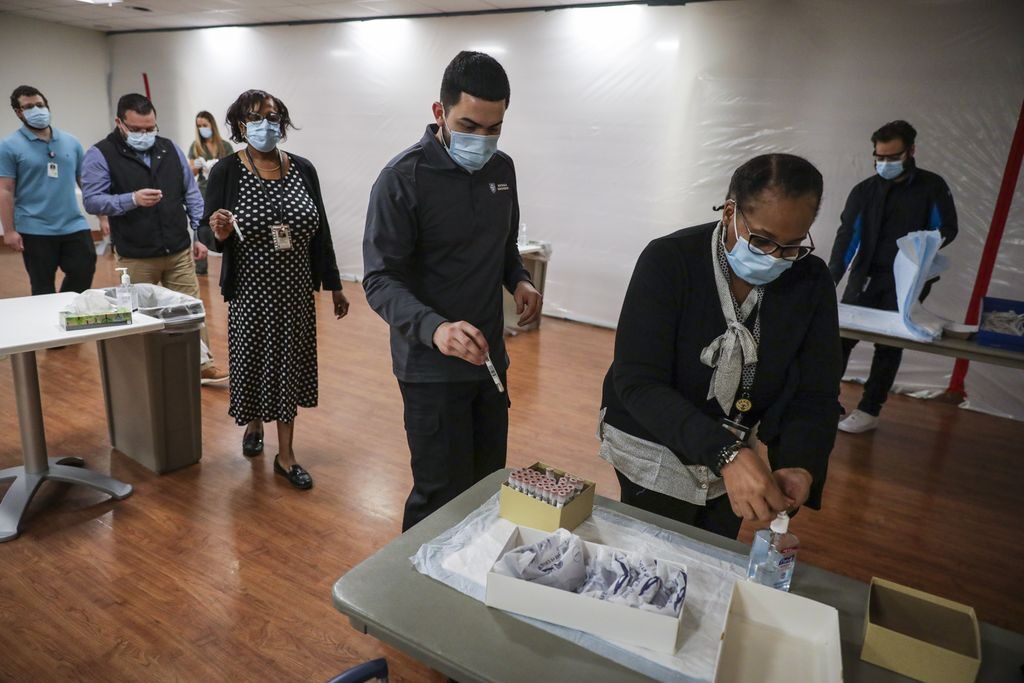
Local hospital leaders have been preparing for a second surge for months, and they’re more confident going into the winter now that they’ve had experience with COVID-19 and time to stock up on protective gear, medical equipment, test kits, and drugs.
“We are stronger now than we were then because of fighting through that first wave,” said Dr. Kevin Tabb, chief executive of the Beth Israel Lahey Health hospital system. “But I don’t want to sugarcoat it: We still face some pretty significant challenges. The burden of responding to COVID is monumental for the people that do it on a daily basis.”
Massachusetts hospitals had admitted 705 COVID-19 patients as of Saturday, far below the 3,965 patients hospitalized at the last peak in April.
Dr. Paul Biddinger, head of emergency preparedness at Massachusetts General Hospital and the Mass General Brigham hospital system, said internal models predict a modest rise in hospitalizations, not the sharp climb seen in the spring. The models don’t yet indicate exactly when the next peak will occur, or how big it will be. But the increase in hospitalizations should remain slow and steady if people continue wearing masks and keeping distance from others.
“We hope that a second surge will be less than what we went through in the first — ideally, dramatically less, but that requires us all to continue to follow restrictions,” Biddinger said.
“What we are all afraid of is changes in public behavior over the holidays, especially because of Thanksgiving, Christmas, New Year’s, [and] there are lots of people who are indoors with families, without masks,” he said. “That really is a very significant risk for substantially changing community transmission, which would really accelerate the surge that we’ve seen.”
For now, hospitals are not planning widespread cancellation of routine appointments and procedures to make room for COVID-19 patients as they did in the spring, under direction from the state. Governor Charlie Baker said last week that state officials are “doing everything in our power to avoid that scenario happening again.”
Tabb said Beth Israel Lahey could cancel procedures to free up more hospital space in 72 hours if need be. “We’re constantly watching, adjusting, and changing,” he said.
After a lull in COVID-19 cases over the summer, hospital leaders have resumed regular communication with one another,and say that if cases rise precipitously again, they will work to balance the burden across Boston and the state so that no single hospital becomes overwhelmed.
If needed, they say, they again can add ICU beds and redeploy doctors and nurses. State officials also are planning to set up new field hospitals, as they did earlier this year to manage the potentialstrain on the health care system. The first will be at the DCU Center in Worcester, which functioned as a field hospital in the spring, and will be available for patients again the first week in December.
Another big change:This time as cases rise, an effective vaccine may be in sight — and distribution could begin in time to combat the winter surge, said Dr. Eric Dickson, chief executive of UMass Memorial Health Care, which was a test site for the Pfizer vaccine candidate.
“It’s this race to keep the transmission rate low enough that we can manage the care while we work to get the vaccine done,” Dickson said. “I think we’ll be vaccinating people in January.”
Massachusetts hospitals also have spent the past several months building up their stores of personal protective equipment and are not as desperate for masks and other supplies as they were in the spring — though health care facilities in other states are scrambling to find enough protective gear.

The Mass General Brigham system, for example, purchased 39 additional ventilators and stocked up on protective gear, going from a two-week supply in the spring to a four-month stockpile now, officials said. Boston Medical Center also has gone from counting its supply of protective equipment in days, to months, and has collected a year’s supply of the hardest-to-acquire items, according to chief executive Kate Walsh.
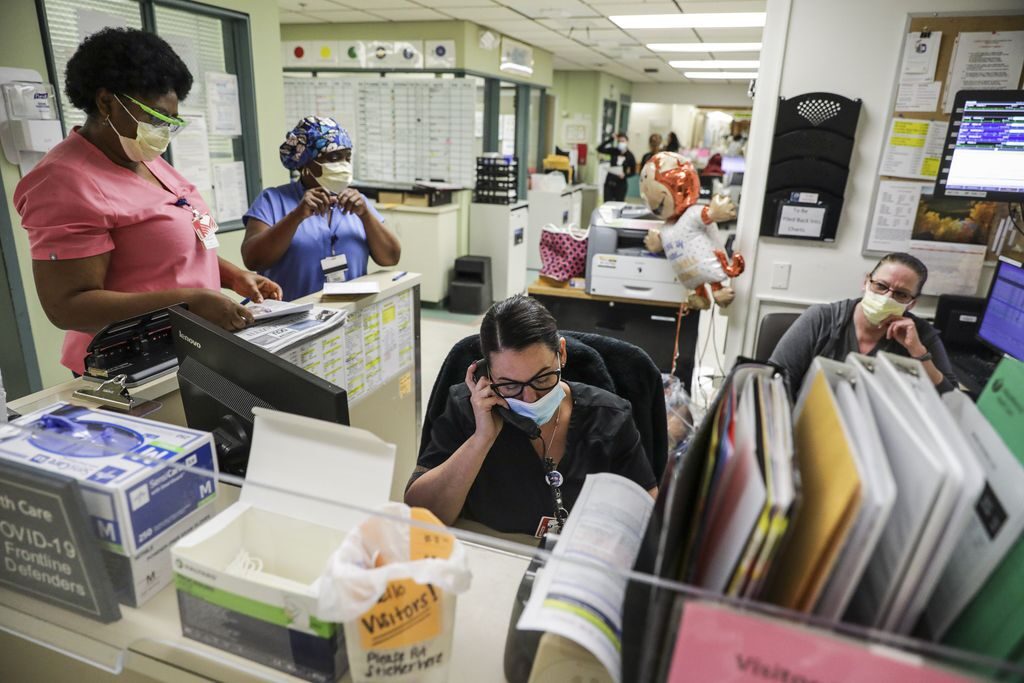
But sincehospitals plan to continue treating their regular patients even as COVID-19 cases rise, they must double down on infection control and carefully manage patient flow to prevent overcrowding.
“The real challenge that we’re wrestling with now is not just COVID coming back, but continuing to deliver care for non-COVID patients,” said Dr. Alastair Bell, chief operating officer at Boston Medical Center.
Another potential hurdle: Hospitals may see a rise in patients with seasonal flu along with the rise in COVID-19 patients, and distinguishing between the two illnesses can be tricky because the symptoms are similar.
“We may see a lot more patients with COVID-like symptoms,” said Dr. Charles Morris, associate chief medical officer at Brigham and Women’s Hospital. “That’s another demand, another stressor.”
And there is growing fatigue among the general public, with people tired of wearing masks and keeping their distance from friends and family, and among front-line health care workers still reeling from the punishing days of last spring when they feared for their own safety as they battled an unknown disease. Those factors could all come to a head with the holidays and cold weather coming.
“We’re more confident, we’re more experienced,” said Dickson, of UMass Memorial, “but for the most part people are more tired.”

