Jerome Groopman, MD (Experimental Medicine, BIDMC) writes about the timing of research regarding COVID-19 and the importance of its quality.
New Yorker – July 23, 2020
The Long Game of Coronavirus Research
Last month, Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases, spoke at a biotech conference, where he emphasized how much is still unknown about the coronavirus. “I thought H.I.V. was a complicated disease,” he said. “It’s really simple compared to what’s going on with COVID-19.” To anyone who knows the history of AIDS research—Fauci has spent much of his career studying the disease—this was a dismaying thing to hear. In 1984, President Reagan’s Health and Human Services Secretary, Margaret Heckler, said, “We hope to have a vaccine ready for testing in about two years.” Almost four decades later, there is still no vaccine. If Heckler’s words now seem like wishful thinking, the Trump Administration has worried scientists and physicians with what may prove to be a similar overpromise. In May, it unveiled a plan to deliver “hundreds of millions of doses” of a COVID-19 vaccine by the end of this year. The plan’s name—Operation Warp Speed—is meant to spark hope. But, in science, true hope is clear-eyed and brings a tight focus on the barriers and potential setbacks that exist along the path to desired results.
In the face of a crisis as urgent as COVID-19, speed is desirable, and the worldwide mobilization to conquer the virus has been inspiring. But what Fauci said illustrates why it’s a grave mistake to favor speed at the cost of rigor. Quite simply, this is a disease that we are only beginning to understand: since the outbreak began, it has become evident that its effects are, like those of AIDS, astonishingly diverse and complex. Still largely thought of as a respiratory disease—it can indeed inflict devastating damage to the lungs—it is actually, as Fauci noted, capable of roving throughout the body. There are cases in which it causes kidney failure, stroke, or a so-called cytokine storm, an overreaction of the body’s immune system that can lead to multiple organ failure. In children, infection can lead to multisystem inflammatory syndrome, a condition that can damage the heart and other vital organs. COVID-19 has a startling spectrum of severity—from no symptoms to death—depending on a host of poorly understood factors. Fauci also pointed out another unknown: whether some survivors, especially those with the severest symptoms, would end up dealing with lifelong debilitating effects. Currently, we are not even sure how to assess protective immunity if we had a vaccine in hand—whether protection would be broad among all age groups and encompass the healthy as well as those whose clinical conditions, such as diabetes, heart disease, and obesity, predispose them to COVID-19. Even more worrying, for those who imagine a vaccine might end the pandemic like turning off a light switch, a number of recent studies suggest that people who’ve had the disease may not emerge with robust, lasting immunity. If so, it’s possible that the initial protection offered by a successful vaccine would similarly wane, and people could be infected again.
It’s understandable how desperate we all are for quick solutions, with the number of infections and deaths skyrocketing. Some twelve hundred clinical studies have been designed since January, but many are too small to have much chance of producing clear results. Researchers have been publishing their papers online before they have undergone peer review. In May, the biotech company Moderna published initial results of an early trial of their vaccine in a press release. Moderna’s vaccine dominated research news again last week, after fuller results of that trial were published in The New England Journal of Medicine. That work is still a preliminary achievement, since there were only fifteen healthy volunteers in each of three vaccine dose groups, and, in the moderate- and high-dose groups, almost every volunteer had side effects. An accompanying editorial from Penny Heaton, of the Gates Foundation, cautioned that we won’t really know about the safety of Moderna’s vaccine until many thousands receive it, nor whether the reported immune response in volunteers is actually protective against the virus. There are clear risks with proceeding to human trials in haste. As Kenneth Frazier, the C.E.O. of Merck, pointed out last week, there have been cases, in the past, in which trial vaccines “not only didn’t confer protection, but actually helped the virus invade the cell, because it was incomplete in terms of its immunogenic properties.” Promises to have a vaccine ready by the end of the year, he said, did a “grave disservice to the public.”
Producing a vaccine that is able to confer immunity on disparate age groups with varying levels of vulnerability is an enormous task, especially because COVID-19 is a brand new disease in humans, and therefore one to which we have no natural immunity. (Even a vaccine as comparatively simple as the annual flu shot reduces the risk of flu sickness for only about forty to sixty per cent of recipients.) All this means that a first vaccine, while a welcome tool in fighting COVID-19, may well turn out to be of limited use. The lesson learned from AIDS is the value of building a protective scientific infrastructure beyond a vaccine, something that requires legions of scientists working carefully and in concert to understand the numerous ways that a virus causes disease.
In early June, I visited the National Emerging Infectious Diseases Laboratories (NEIDL), to interview researchers there who are working on COVID-19. Part of Boston University, NEIDL (pronounced like “needle”) is one of two academically-affiliated institutions in the U.S. with laboratories that are certified to handle the deadliest pathogens known to man, like the Ebola and Marburg viruses and yellow fever. NEIDL’s origins date to the period after 9/11, when Fauci warned that the country needed a better system to defend against possible bioterrorism attacks, and the government earmarked billions of dollars to prepare for such an event. NEIDL received its funding in 2003, but getting a facility ready to handle such pathogens takes years: the building itself was completed in 2008; acquiring the necessary environmental approvals from local government and community representatives took almost a decade. It wasn’t until 2017, that NEIDL was fully approved to undertake all the work for which it was created.
The facility, which is on B.U.’s medical campus, in Boston’s South End, stands seven stories high, a modern structure of glass and concrete. Barriers surround the site at a distance of a hundred and fifty feet from the building; they are fitted with motion-detection sensors and are strong enough to stop a fifteen-thousand-pound truck going fifty miles an hour. Inside, there are around a dozen containment laboratories for dangerous microbes, which hold specialized microscopic equipment and robotic devices, and secure environmental facilities designed for pathogen vectors, like mosquitos and ticks, and animals, which researchers use to model human diseases. NEIDL’s Biosafety Level 4 facility—the part of the building that is licensed to handle the most dangerous microbes—is constructed as a building within the larger building. That nested structure has twelve-inch-thick concrete walls coated with multiple layers of epoxy resin. While NEIDL itself is built on piling that go into bedrock, the B.S.L.-4 floors are flexible, and can move at a different frequency from the main structure in case of an earthquake. Researchers work in sealed suits, resembling those of astronauts, with a large transparent bubble over the head, supplied with filtered air via a hose connected to the ceiling. If there is a spill, the space is typically decontaminated with chlorine dioxide, and low air pressure maintained in the lab insures that air rushes in rather than out, so that no airborne virus can escape.
NEIDL has been working with live samples of the coronavirus since March, when it received a sample that was derived from the U.S.’s first diagnosed case: a thirty-five-year-old man in Washington State who had recently returned from Wuhan. But its staff had been making plans to investigate the virus since January, when early reports of its rapid spread convinced them that it would proliferate worldwide and lead to severe outbreaks in the U.S. They immediately began writing protocols for using the virus and submitting requests for approval from B.U. In March, institutions at B.U., including NEIDL, received 1.9 million dollars in funding from the Massachusetts Consortium on Pathogen Readiness, part of a hundred-and-fifteen-million-dollar grant—coördinated by the Dean of Harvard Medical School and financed by a Chinese investment fund—to support researchers working in the Boston area and Guangzhou.
In the U.S., most of the B.S.L.-4 labs are in government or military facilities, but NEIDL, despite its origin as part of a federal initiative, operates on an open academic model. “We work with absolute transparency,” its director, Ronald Corley, told me. “We have to have the trust of the public, so everything we do is known and communicated freely.” In the past two years, Corley, a lanky microbiologist in his seventies, has recruited fourteen scientists to join the center, looking for researchers with a wide range of expertise. The staff of NEIDL and its affiliates includes experts in the basic biology of the deadliest pathogens, in animal models that can be used to mimic the progress of human diseases, and in effective treatments and potential vaccines. Corley believes in giving them the freedom to pursue their hunches without being micromanaged. From the outset, he organized the center’s COVID-19 research on the presumption that it would be, as recent evidence has borne out, an evolving target—and that progress would more likely come from a cluster of approaches than from a single breakthrough.
Since Donald Trump took office, his Administration has worked to systematically disassemble key elements of federal pandemic planning. In 2018, it largely disbanded the National Security Council unit responsible for pandemic preparedness, which was formed during the Obama Administration, after having ignored the council’s playbook for fighting pandemics. It removed Rick Bright, from his job as a Health and Human Services official in charge of vaccine development, after he submitted a three-hundred-page complaint about the Administration’s coronavirus response. Most recently, the White House directed the National Institutes of Health to cut off federal grant funding to the EcoHealth Alliance, an organization headquartered in New York that studies the global spread of viruses from animals to humans, and which collaborated on research about coronaviruses with researchers based in China.
But some aspects of the country’s pandemic planning have managed to survive, in large part because they were designed as enduring homes of scientific inquiry into the most dangerous biological threats. NEIDL was conceived to be at once independent of politics and ready to respond in a cohesive way to a national emergency. Its approach represents the polar opposite of the “warp speed” language popularized for the public.
“There’s lots of good work going on across the globe,” Corley said. “There’s also a lot of junk, because people are rushing.” The issue is not just sloppiness; laboratories are inherently artificial environments, and even the most careful work can yield apparent breakthroughs that turn out to be artifacts of the experimental process. When a virus infects human cells grown in a lab, it can mutate slightly. It is possible to spend years developing a therapy for an altered form of a pathogen only to find that that therapy brings no benefit to patients. Corley and his team have been sequencing the genes of their virus samples repeatedly as they work, in order to make sure that the pathogen is not morphing into a form that no longer corresponds with what was originally retrieved from the Seattle patient—a time-consuming, but necessary, precaution.
As Corley led me on a tour of the facility and introduced me to its researchers, I got a sense of NEIDL’s institutional preference for care over speed. Anthony Griffiths, a virologist and an Ebola expert whose focus is on animal modelling, stated the value of deliberate science plainly. “I learned lessons from Ebola. I understand speed,” he told me. “But, if you do science in a rush, you are at risk of going down the garden path.” Griffiths hopes to use observations of the progress of the disease in animal hosts—genetically manipulated mice, golden Syrian hamsters, and rhesus monkeys—to learn about its mechanisms and to test possible treatments. This could help determine how much virus has to be present to cause infection, and what the routes to inoculation might be, with the aim of uncovering the dynamics of human immunity against the coronavirus. “I would love to be first, but we’re not going to be,” he told me. “But we want to put ourselves in the best position to do the kind of work that can help understand the performance of the vaccine, and what its limitations may prove to be.”
Griffiths works closely with Nahid Bhadelia, an infectious-diseases physician at Boston Medical Center who is an expert in emerging pathogens. In 2014, during the Ebola outbreak in West Africa, she was part of a W.H.O. team that treated patients and training local caregivers. Part of her role is to draw the attention of NEIDL scientists to evolving and unexplained clinical findings of COVID-19, such as those that Fauci highlighted, so that they investigate them in the laboratory. For example, she has observed patients who tested positive for SARS-CoV-2, the virus that causes COVID-19, then repeatedly tested negative, and then tested positive again. “Have they become reinfected or has their immunity waned?” she said. “Or were they just shedding virus from the initial infection?” With scientists at NEIDL, she is working to take a chronological sequence of virus samples from such patients. Genetic analysis can show whether a patient was carrying the same pathogen at different times, or whether the virus mutated in a way that outflanked the person’s immune response. This work will ultimately make it easier to assess the likely potency of prospective vaccines. Bhadelia has also noted that some patients who were “not terribly sick, meaning they weren’t in the I.C.U,” nonetheless appear to have residual problems with cognition. Such persistent effects could potentially be modelled in animal studies at NEIDL.
Rob Davey, an Australian microbiologist with a wry sense of humor and hyperkinetic way of talking, is an expert on discovering novel treatments for pathogens. In 2018, while he was working with the biotech company Regeneron, Davey helped identify a kind of antibody that successfully treated Ebola in animal test subjects by latching onto viral proteins and blocking the microbe from entering cells. These antibodies ultimately became treatments for patients with the infection. Since he began working on COVID-19, he has been looking for agents with the potential to disrupt the progress of the disease. He is currently screening almost seven thousand chemicals that he obtained from the Broad Institute (the joint Harvard–M.I.T. enterprise that specializes in assembling large libraries of chemical compounds), along with an additional thirty-two hundred provided by B.U. Some of these compounds are drugs already in use for illnesses including diabetes, hypertension, and migraine. If Davey’s screening process indicates that one of them has potential as a COVID-19 treatment, testing on patients could follow quickly, since they already have F.D.A. approval.
To screen so many compounds, Davey uses a robot to dispense carefully calibrated microlitres of compounds into batches of tiny plastic wells containing cells that have been exposed to the virus. A green fluorescent marker is used to indicate SARS-CoV-2 within cells; if the color is reduced, a compound has been able to stop the virus reproducing. So far, Davey told me, the hit rate has been 2.5 per cent, which is quite high. “Now we have to go back and assess which of these could be treatments,” he said. Virtual 3-D modelling of molecules makes even greater efficiency possible, at least for a preliminary screening. Davey has been working with Haribabu Arthanari, a biophysicist at Harvard Medical School, who has led a project to screen by computer the structures of billions of chemicals, at least three thousand of which turn out to be the right shape to fit into key parts of the coronavirus, making them promising subjects for laboratory study.
Such collaborations with the wider research community are pivotal to the way NEIDL operates. Elke Mühlberger, a German virologist who is an expert in the study of the Ebola and Marburg viruses, has been using her lab at NEIDL to perform SARS-CoV-2 infection studies for more than a dozen scientists at institutions across Massachusetts. Even before the outbreak, she was collaborating with Darrell Kotton, a specialist in pulmonary medicine and critical care who is the head of B.U.’s Center for Regenerative Medicine, on a technology he has developed that, fortuitously, has exciting implications for COVID-19 research. Using stem cells, he has been able to grow a kind of human lung cell known as a type-II pneumocyte. These cells, which Kotton likens to soccer balls, appear to be a primary target of SARS-CoV-2, but they haven’t previously been available for experimentation in significant quantities: they live deep in the lung’s alveoli and can’t be retrieved except by means of major surgery.
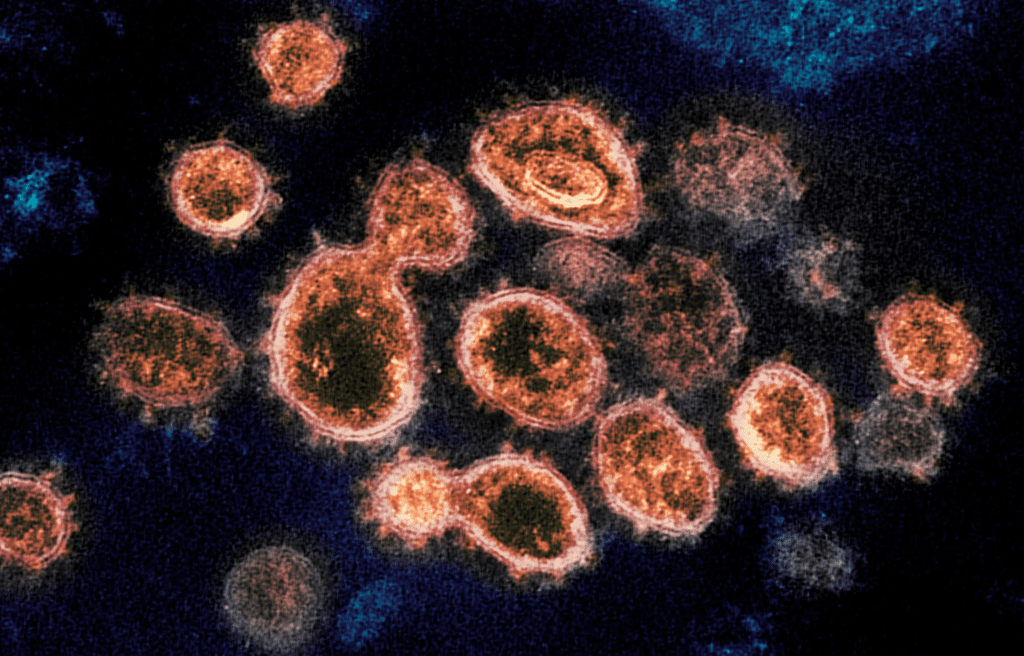
Kotton has been struck by the dramatic demise of some COVID-19 patients whom he cares for in the I.C.U. “They had had nothing more than what you would call a cold, with some fever and sniffles, but then, after a week or so, and in a matter of hours, they would crash,” he told me. “And I asked myself, What the heck is going on in the lung? Now we can study the type-II pneumocyte over time. We have in the lab the cells that can tell us what’s going on.” At NEIDL, I saw photographs from Mühlberger’s lab of some of these cells being infected with SARS-CoV-2. To monitor the virus, it was stained with a green fluorescent antibody; after the individual cells were packed with virus, they became glowing green globs. These cells, Kotton believes, can provide a way to observe the behavior of the virus in its first interactions with its primary target in the lung. “It’s taken me fifteen years to grow it in the lab,” he said. Now researchers all over the world were calling, asking if he could provide them with cell cultures to use in their work.
Science is an iterative process, in which each stage builds on the successes and failures of the last. Surveyed collectively, the multifarious initiatives based at NEIDL seem like disparate enterprises. But assembling a picture of the coronavirus requires pursuing many parallel lines of inquiry, while also assimilating existing medical knowledge. My own laboratory has worked on endothelial cells—the cells that line the body’s blood vessels and serve as a barrier against the entry of pathogens—for years, as part of an effort to ameliorate the effects of H.I.V. In the past few months, evidence has emerged that suggests that these cells are also a major target of the coronavirus. A group of researchers recently published findings showing viral particles in the endothelial cells of the frontal lobes of an Italian coronavirus victim, which could potentially explain some of the virus’s neurological effects. Other research has also suggested that they play a significant part in many other of the most dangerous effects of the coronavirus, like kidney failure, stroke, and the inflammatory illness reported in children. Our lab is now working to decipher how the virus may carry out such attacks on endothelial cells, with the aim of identifying ways to prevent them.
Modern medical research is inherently collaborative, but the constellation of efforts now under way around the world is unprecedented in scale and scope. That diffusion heightens the value of places like NEIDL, which acts as a hub of knowledge. Many facilities fulfill a few of the functions that NEIDL does, but few gather so many disciplines and approaches under one roof, and fewer still also make it part of their missions to proactively pursue collaborations with surrounding institutions. This is no accident but, rather, a testimony to the value of long-range thinking, even at those moments of crisis when speed is on everyone’s mind. As Corley showed me around, he reminded me of the fact that the reason NEIDL had a diverse but integrated team of researchers at the ready to study a catastrophic viral outbreak was the foresight of Anthony Fauci’s recommendations after 9/11. “COVID was the raison d’être for creating NEIDL,” Corley said. “The pandemic fulfills its mission.”

