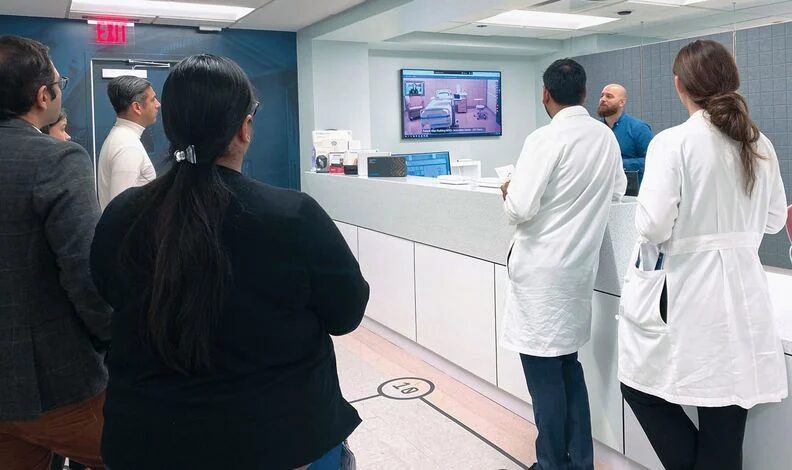
During Modern Healthcare’s Transformation Summit webinar series, Kevin Tabb, MD (President & CEO, BILH) discussed the collaboration and partnerships between local hospitals during the COVID-19 pandemic.
Modern Healthcare – May 23, 2020
Next phase of telemedicine to move beyond video visits
In the wake of COVID-19, Modern Healthcare moved its annual Transformation Summit online. The five-part webinar series brought together healthcare and technology leaders to discuss topics like innovation in times of emergency, patient-centered care and mental health.
The rapid spread of COVID-19 across the U.S. may have given telemedicine adoption a kick forward—but video visits alone don’t capitalize on the possibilities of remote care.
In response to the outbreak, hospitals have been ramping up their use of telemedicine as a way to let patients receive care at home. At CHI Franciscan, part of CommonSpirit Health, physicians are now conducting almost 1,500 virtual patient visits per day. Before the pandemic, that number was closer to 20 daily visits.
“I really believe, coming out of this, that is something that we’re going to truly double-down on,” said Ketul Patel, CEO of CHI Franciscan and president of CommonSpirit’s Pacific Northwest division, during a session that was part of Modern Healthcare’s Transformation Summit webinar series.
A shift to more care being delivered remotely will be bolstered by new devices that help physicians collect patients’ clinical data from afar, said Roberta Schwartz, executive vice president and chief innovation officer at Houston Methodist.
Although hospitals have seen a sharp rise in telemedicine use with the outbreak, she suggested telemedicine will experience a dip once facilities can reopen for non-emergent care.
That dip could be driven by numerous factors, including patient and provider preferences, as well as reimbursement barriers. Although CMS has expanded reimbursement for telemedicine during the outbreak, those changes are set to lapse when the public health emergency ends.
That said, Schwartz expects telemedicine use to stay at a much higher rate than it was before COVID-19, especially as technology solutions become more sophisticated.
Dr. Aaron Neinstein, director of clinical informatics at the UCSF Center for Digital Health Innovation, cautioned leaders against feeling locked into video visits as their main strategy, advocating for the role that asynchronous telemedicine options can play alongside video visits and in-person care.
“One of the unfortunate discussions that I hear happening in a sort of binary term is whether we’re going to use in-person care or video visit care,” Neinstein said. Asynchronous communication, however, could build on those two care avenues by using chatbots or automated text messages for check-in and to evaluate a patient’s health between formal appointments with a physician.
“Video (will be) an important component in the future,” he said. “But we have to blend—in a rational manner—in-person care with synchronous video visit care with asynchronous remote monitoring-type care.”

3 thoughts from Google Health VP Dr. David Feinberg
A trained psychiatrist and former CEO of Geisinger Health, Feinberg discussed mental health in the time of COVID-19. Here are three highlights. The following quotations were edited for clarity.
1) Why Google Search is tech’s biggest healthcare success
When I started as a doc I—and I say this with quotes—“I knew everything, the patient didn’t.” They came to me and I had all the information. Google Search started 20 years ago. Now, when patients come in—and we need to work to make sure we get better authoritative information—we’ve leveled the playing field. Now, the patient oftentimes has as much information as I do. Google Search fundamentally changed that doctor-patient relationship.
2) Web screening for mental health conditions
If someone searches, for example, “I’m depressed” or “I want to hurt myself” on Google, then the PHQ-9—a validated screener for depression—comes up. People can answer nine questions about how their mood state is, and get feedback on whether they screen mild, moderate or severe for depression, as well as information about what to do as far as the next steps. With mental health, there’s so much delay between when people start suffering and when they tell any other human being. We think by getting great information, authoritative information, out there in good screeners we can actually decrease the time of suffering.
3) On Google’s need to earn healthcare’s trust
I’m absolutely convinced that Google’s technology could save lives. I’m also equally convinced that if we don’t earn the trust, all this stuff will never make it out of Google. It’s got to be established on a very trusting relationship that’s transparent, dignified, culturally sensitive, equitable and understandable. We have to keep earning it, we have to keep demonstrating it, and then, at the end of the day, our products have to be so helpful, so useful, so clear that even the biggest skeptics would say, “You know what, this is making my life better.” New partnerships integral to COVID-19 response
The novel coronavirus, according to Dr. Kevin Tabb, CEO of Beth Israel Lahey Health, is like a fire spreading through an apartment building: It’s not enough to save your own unit, because it’s a group problem.
“If you put out a fire in your apartment but the ground floor burns down, you’re going to be in trouble,” Tabb said during a session at Modern Healthcare’s Transformation Summit webinar series. “This virus, this crisis, does not respect boundaries. We need to find ways to work together.”
That meant not only working more closely with other leaders within the Cambridge, Mass.-based system, but also with the six competing academic medical centers and three medical schools across the greater Boston area, not to mention other providers throughout the state.
Since the start of the COVID-19 crisis, leaders from many of those competing hospitals have participated in daily calls with one another and local officials, including the governor of Massachusetts and the mayor of Boston, where they discuss challenges and solutions. That’s led the organizations to better distribute patients, personal protective equipment and ventilators during respective surges and shortages.
“We began to talk, to coordinate and to help each other in ways that I’ve never seen,” Tabb said.
That need for collaboration has been a common reaction among hospitals across the nation.
“It’s very interesting how the sense of urgency changes when people can rally around a common enemy,” said Teri Fontenot, CEO emeritus of Woman’s Hospital in Baton Rouge, La.
In response to COVID-19, Kaiser Permanente set up command centers in each of its nine regions—eight states and Washington, D.C. Each command center is led by an incident commander from Permanente Medical Group, alongside a colleague from Kaiser Foundation Health Plan or Kaiser Foundation Hospitals.
The regional command centers manage the response for their specific area, as well as participate in daily virtual huddles with Kaiser’s national command center. That collaboration has helped the Oakland, Calif.-based organization improve resource allocation.
“When you collaborate across a broad spectrum of hospitals, the overall product improves,” said Dr. Richard Isaacs, CEO and executive director of the Permanente Medical Group and co-CEO of the Permanente Federation.

