A new study authored by James Kirby, MD (Pathology, BIDMC) and others shows that decontamination of N95 masks for reuse can be done safely with simple tools.
Fast Company – June 26, 2020
How to decontaminate an N95 mask in just 3 minutes
Months after mask manufacturers ramped up production of N95 masks in response to the coronavirus crisis, hospitals, clinics, and nursing homes taking care of COVID-19 patients are still facing shortages of the respirators. Because of the lack of supply for essential workers, consumers still can’t buy the masks in many stores, despite the fact that they’re one of the best lines of defense against the virus. And as COVID-19 cases spike in many areas, the problem will get worse.
The masks are only designed for a single use. But a new study shows that they can be safely decontaminated for reuse with simple tools. While only some hospitals have fairly expensive disinfection and sterilization equipment, the process tested in the study could be used anywhere. “Not all people who have need of an N95 mask necessarily have access to these industrial-scale disinfection processes,” says James Kirby, a professor of pathology at Beth Israel Deaconess Medical Center, a teaching hospital at Harvard Medical School, and one of the authors of the study.
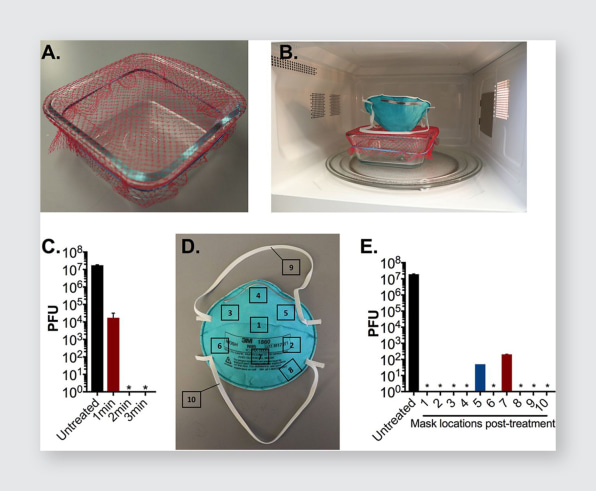
The researchers tested an approach that uses steam generated in a microwave. Steam isn’t a new method for disinfection, but it typically involves using commercial steam bags—they’re also in short supply right now. The new method uses only commonly available household supplies. In the study, the researchers used a rubber band to attach mesh from a produce bag to a glass container, filled the container with water, and then placed a virus-doused N95 respirator on top of the mesh. The mask was coated in MS2 phage, a virus that is harder to kill than the new coronavirus because it has a tougher outer coating, meaning that anything that destroys it will definitely work on SARS-CoV-2. The dose of virus was also higher than what a healthcare worker is likely to encounter. “It was a good surrogate in that we could carefully quantify sort of the viral killing, if you will, and that allowed us to basically find the sweet spot for sort of the minimal amount of microwave time to reliably disinfect or inactivate this particular virus,” Kirby says.

They also tested a few variations, including suspending the mask over a ceramic mug (this worked, but didn’t fully decontaminate the straps) and putting the mug inside a Ziploc bag to concentrate the steam (the bag melted, and the method risked burning the person trying to retrieve the mask). But the glass container—the same type of simple container used to store food—worked perfectly. After three minutes in a standard 1,110-watt microwave, the steam from the water had killed the virus. And even after repeating the process 20 times, there was no change in the fit or function of the mask.
Of course, reusing masks that were never designed for reuse is still less than ideal. There are caveats—the researchers didn’t test whether wearing the masks 20 times in a row leads to a loss of quality, like whether the straps stopped working, for instance. But the tests found that the decontamination process didn’t make them degrade or make them less effective at filtering the virus. They also tested only one type of mask, meaning that there might be variations in masks from other manufacturers. But for those with no good option, like the hundreds of nursing homes that have reported running out of masks, a proven method of decontamination is better than relying on inadequate surgical or cloth masks—or nothing at all. As of this week, an estimated 697 healthcare workers have died from COVID-19 in the U.S. alone because they didn’t have enough protection.

