Molly Hayes, MD (MICU, BIDMC) and Pamela Peck, MD (Clinician Health Services, BIDMC) share that as COVID-19 cases in Massachusetts are declining, many health care workers are reflecting on their difficult experiences over the last few months and will need support from their institutions and communities.
WBUR – June 22, 2020

‘Invisible Wounds’: Frontline Health Workers Face Recovery Period That Could Last Months
Dr. Molly Hayes says she doesn’t feel exhausted.
“Honestly, I don’t feel physically tired,” she says, “but it just feels like sort of a let-down.”
As director of the Medical Intensive Care Unit at Beth Israel Deaconess Medical Center, Hayes worked nearly nonstop through the thick of the COVID-19 outbreak. Now, she says, she’s not depressed, but “it feels weird. For three months we were all systems go almost 24 hours a day. And then it just felt like one day you woke up and… there were no texts. And you didn’t hear from anyone.”
Although the number of new coronavirus cases in Massachusetts has been steadily declining, there’s still plenty to do right now getting the unit back to normal and figuring out lessons learned. And staffers who worked long stints at the peak of the crisis are taking time to rest, Hayes says, “so they’re home with their families now, and sort of recharging and refreshing, and then they’ll be ready for the fall surge.”
At least, that’s the goal: to recover enough to face down the virus again if need be.
Retired Brigadier General Jack Hammond sees a parallel between the COVID-19 front line in hospitals and a military deployment.
“This is not dissimilar — when you see thousands of people die in very rough ways, in a very chaotic environment, and then suddenly it’s over,” he says.
Hammond led troops in Iraq and Afghanistan. Now he leads Home Base, a Massachusetts General Hospital program that treats veterans with brain injuries and Post-Traumatic Stress Disorder, and he oversaw the thousand-bed Project Hope, a temporary field hospital set up in in Boston to serve coronavirus patients at the height of the outbreak. He says the adrenaline is gone now for frontline staffers.
“And so when they have time to reflect upon some of the things that they witnessed and experienced, that’s when it’s probably going to affect them the most,” he says. “Because in the heat of the moment, they may have a quick cry in a bathroom and then they’re back on the floor, helping somebody else.”
He says these workers can be left with invisible wounds much like veterans.
“We’ve now got wounded health care warriors that are coming out that are going to need the same type of care,” he says. “It won’t all be post-traumatic stress disorder, that level, but there’ll certainly be post trauma stress.”
It’s critical for health care institutions to provide support, he says — and for staffers to be willing to seek help. Local hospitals all have employee support programs, but “the challenge, just like our soldiers, is getting people to participate in them,” he says.
Hammond expects some frontline workers to grapple with anxiety and depression. Some may also have trouble sleeping and concentrating, a lack of pleasure or a feeling of hopelessness, says psychologist Pamela Peck, the director of the Clinician Health Service at Beth Israel Deaconess.
“Other folks may be suffering from a sense of isolation or numbness, a sense of detachment,” she says. “That’s what we often see in folks suffering from acute stress.”
The spectrum of other possible symptoms includes substance use issues, personal conflicts and irritability. “And those will be more prevalent after the event, in the next three months, I would imagine,” she says. “This is what we’re going to be watching out for.”
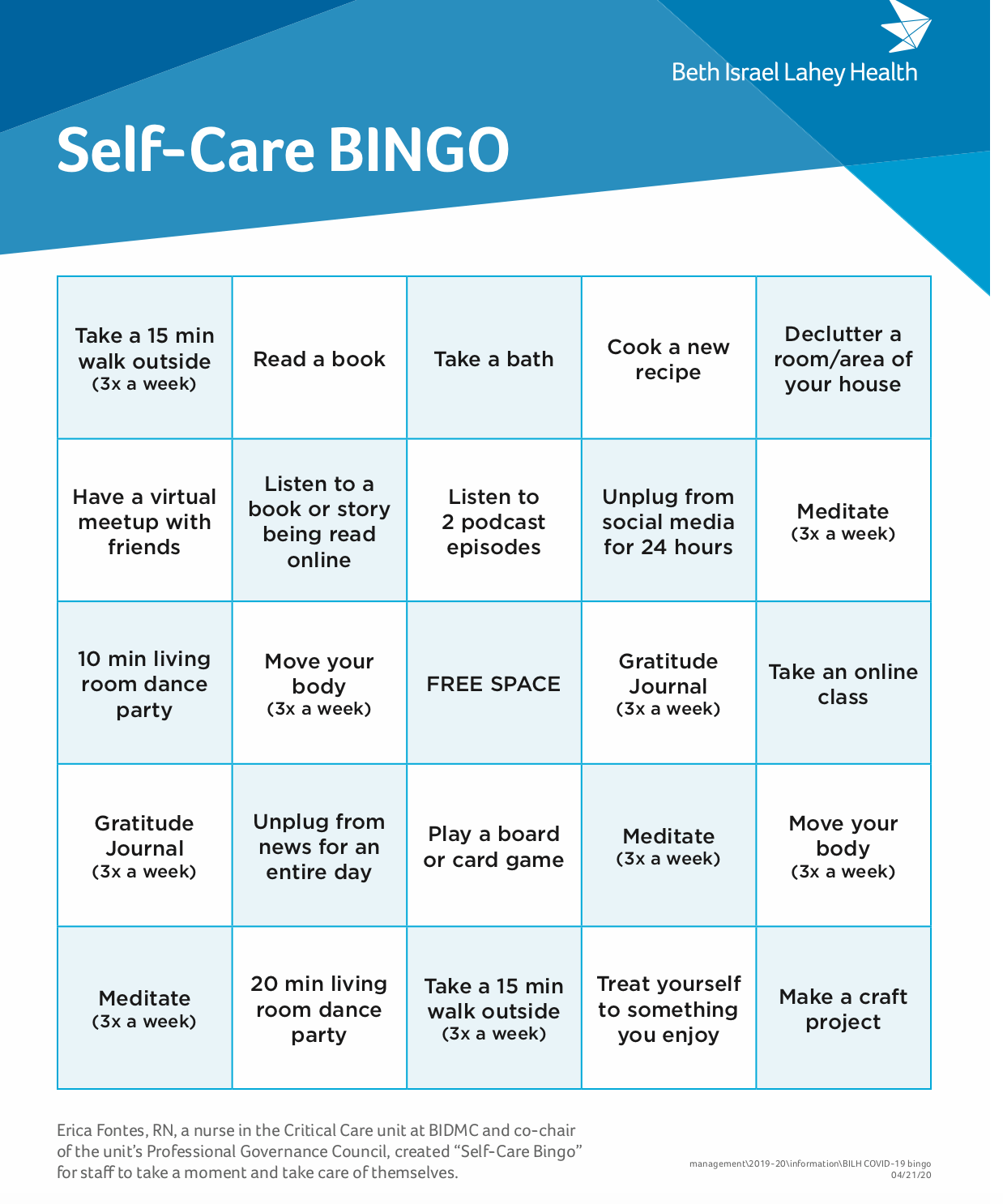
She and others say self-care can help — sleep and exercise, good nutrition and time with loved ones — and so can communal support to acknowledge the losses caused by the pandemic.
“Will we recover in time to be ready for the next piece that life brings us? I think many people will,” Peck says. “But I also think that it requires communities and individuals to gather emotionally around the recognition of how hard this has been.”
And how hard it continues to be, as the post-surge pandemic lingers. There’s no hard and fast rule about how long it will take health care workers — and regular folks — to feel more normal and less exhausted, Peck says. That depends on multiple factors, like your personal history and the intensity of the stress you’ve just been through, and the baseline level of stress you started from.
The National Academy of Medicine estimated three years ago that about half of doctors suffered from symptoms of burnout, including fatigue. And it’s not only doctors.
“One-quarter of ICU nurses, as an example, had symptoms consistent with a clinical diagnosis of Post-Traumatic Stress Disorder,” says Dr. Darshan Mehta, the medical director of the Benson-Henry Institute for Mind Body Medicine. And the pandemic has surely taken a major toll far beyond previous levels, he says.
Mehta uses a personal rule of thumb for how long it takes to recover: “If you’ve been working for a period of time, like four weeks, it will take that many months to recover. There is no evidence to back that up, but I think we need to be extremely patient.”
General Hammond from Home Base says active duty soldiers usually get a block of leave — a full 30 days off when they come back from a tour of duty. But members of the National Guard and the Army Reserve often have to dive right back into the job and life they’d left behind — and that lack of a break could be an added challenge for many health care workers now too, including some of the 700 who worked at Boston Hope, he says.
Boston hospitals are actively planning for a possible new surge in the fall or winter. Dr. Molly Hayes from Beth Israel Deaconess says the preparation feels different from before this first wave.
“I at least had some little glimmer, like ‘Maybe we’re not going to get to this, maybe we won’t have to surge. We have to plan, but maybe it won’t happen,’ ” she says. “I’m not thinking that for the fall. I’m just thinking we are going to be there. This is going to happen.”
And whether or not she and her ICU colleagues are fully rested, they will be ready.