David Avigan, MD (Hematology and Hematologic Malignancies, BIDMC) discusses the impact COVID-19 has had on care for patients with cancer.
Los Angeles Times – May 29, 2020

(Dania Maxwell / Los Angeles Times)
Engineer? Cancer expert? Physicist? They’re coronavirus researchers now
It was 2 a.m. on a Saturday morning in March, and Matthew Grayson was exhausted. The coronavirus was reshaping academic life and the Northwestern University electrical engineer had spent the day in his basement office fielding emails from fellow researchers while moving his lecture notes online and familiarizing himself with Zoom.
But as he took one final look through his email before turning in for the night, a request from Dr. Mark Huffman at the university’s medical school caught his eye.
“He said, ‘Matt, you’re an engineer. Can you guys help us with this nasal swab shortage problem?’” Grayson recalled.
Grayson might seem like a surprising choice for such a task — his work usually involves studying electronic materials used in sensors and quantum devices. But now he’s one of a growing army of researchers with no experience in virology who are putting their diverse talents to use to address the COVID-19 pandemic.
For many, the work provides a welcome distraction to the sudden shutdown of their research projects. It also offers a chance to make a difference in a pandemic that has thrown life across the globe into disarray.
Scientists like Grayson have found that even with no experience in medicine, let alone coronaviruses, their skills have proved surprisingly useful.
In his case, the request to work on nasal swabs led him to assemble a group of about a dozen engineers, plus an immunologist and a pathologist.
Public health officials and frontline medical workers have struggled to obtain COVID-19 diagnostic tests. Their efforts have been stymied in part by a shortage of the nasopharyngeal swabs used to collect viral particles from the upper part of the throat behind the nose. Even for those lucky enough to get tested, it can be an unpleasant experience: the long, thin swabs must travel deep into the nasal passage to reach their target.
“People say it feels like stabbing the brain,” Grayson said of the sensation.
Within days of Huffman’s email, Grayson’s group had come up with a design that could be made cheaply (about a penny per swab in materials), quickly (assembled in a minute from readily available components), and efficiently (in lab tests, it collected four times as many particles as the current swabs). On top of that, it would probe only the nasal passage, eliminating that brain-stabbing sensation — and potentially opening the door for widespread at-home testing.
Though his engineering lab has been shut down, Grayson said he’s busier than ever. A patent application for the new swab has been filed, though Northwestern is making the design available for manufacturers to license royalty-free.
“It has been satisfying to feel like you have some agency,” he said of his unexpected project. “But the double-edged sword is that you see the situation unfolding and you’re like, ‘Oh, if only I had skipped another night of sleep, I could have gotten the approvals out earlier and that would have saved umpteen number of lives.’”
Some researchers have gotten into the COVID-19 fight because the disease affects the patients they care for, said Dr. David Avigan, a hematologist-oncologist at Beth Israel Deaconess Medical Center in Boston who researches personalized cancer vaccines.
“It struck close to home in certain ways because cancer patients tend to be among the most vulnerable to the infection and to the potential life-threatening aspects of the infection,” said Avigan, who is in the planning stages of studies to better understand the body’s immune response to the disease. “That created a certain amount of importance and critical meaning for us.”
For those like Albert Nazeeri, a Caltech undergraduate tasked with keeping an eye on the equipment in Joseph Kirschvink’s geobiology lab during the research shutdown, inspiration came from the sudden freeing up of time as nearly all non-coronavirus work came to a screeching halt.

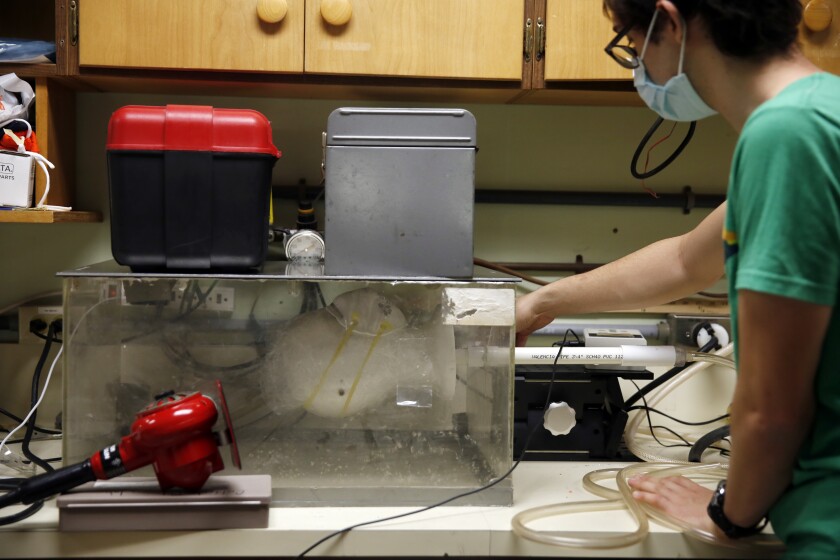
(Dania Maxwell/Los Angeles Times)
Nazeeri was responsible for monitoring the magnetometers, which can measure minuscule amounts of the mineral magnetite in tissues and in rocks, and for checking their cooling systems for helium leaks. It wasn’t particularly taxing, but it dawned on him that simply having access to a lab set him apart from the majority of researchers on campus.
“What can I do? What will be useful?” Nazeeri recalled thinking as he tinkered around the empty lab space.
The physics student had been thinking about the N95 respirator shortage that was leaving hospital workers vulnerable to infection, and he’d been surprised that a potential method for disinfecting and reusing masks — dunking them in a 70% ethanol solution — had been deemed unsuitable because it apparently reduced their particle-filtering abilities.
Nazeeri wondered if that was really true. So he rigged up a laser particle meter to a box containing a Styrofoam dummy head and some plastic tubing. He outfitted the head with a mask and blew air through the tubes and into a chamber to test the mask’s efficacy. Then he dunked the mask in disinfectant, allowed it to dry and ran the test again.
At first, it seemed like the official warnings had been correct — the measurements from the laser particle meter showed that the mask did a significantly worse job of trapping dust particles after it had been disinfected. But then he popped the mask in the lab’s vacuum drying chamber to remove any remaining traces of moisture and found that the mask’s filter was almost as good as new.
“It actually restores them, resurrects them, and it can be done in the poorest clinic in the most rural village in southern Africa,” Kirschvink said. “It doesn’t need major industrial innovations to do it.”
Nazeeri and Kirschvink said that, if replicated by other scientists, the discovery could open the way for a long-overlooked disinfection mode that is fast, cheap and easy for hospitals to perform.
“Serendipitously, we recognized there was a mistake in the literature,” Kirschvink said. “And gosh — maybe we’ll help people.”
The work with masks was something of a side project for Nazeeri and Kirschvink. In other cases, the pivot to coronavirus research has become a full-time job.
(Dania Maxwell/Los Angeles Times)
Dr. David Sullivan usually studies malaria in remote regions of Bangladesh and Africa. That work has made him an expert on the drug chloroquine, which showed apparent promise as a COVID-19 treatment in the outbreak’s earlier days. But after his colleagues at Johns Hopkins University pulled him into COVID-19 discussions, he ended up noticing a research gap in a very different part of the pandemic fight: convalescent plasma.
Plasma is the clear fluid in blood that carries antibodies, the biomolecules the body makes in response to specific infections. Scientists have been testing whether the plasma from COVID-19 survivors can offer some protection against the disease for those vulnerable to it.
Most trials of convalescent plasma are focusing on the sickest patients in intensive care. Sullivan wanted to investigate whether plasma could be used to control the disease much earlier in the process, shortly after someone has been infected.
He likened it to different stages of dousing a fire.
“It doesn’t take much water to put out a match — just a drop — but a drop of water does not do much for a kitchen fire,” he said. “So if we apply this drop of water, the antibodies, early in the disease process, then we can snuff it out and not have downstream damage.”
Sullivan had never run a multi-site clinical trial. It’s meant round-the-clock work and a steep learning curve. But in some ways, he said, it doesn’t really feel like work.
“To me, it’s an existential question right now,” he said. “Society has ground to a halt and I see that this method of convalescent plasma is the way back to a functioning society — and gets me back to working on malaria.”
Focusing on the coronavirus can be something of a salve in tumultuous times — particularly when scientists can’t continue their usual research.
“It is a consolation,” said Dr. Gay Crooks, a developmental immunologist and stem cell biologist at UCLA. “It would be awful to be sitting, waiting to do something useful.”
She and Dr. Christopher Seet, a UCLA cancer researcher, usually work on techniques that could harness the body’s immune response to attack cancer cells, potentially reducing the need for harsh treatments such as radiation and chemotherapy.
Thanks to COVID-19, they’ve found that much of what they’ve learned about the body’s army of infection-fighting T-cells in a cancer setting applies to viruses as well.
“I hope we really make meaningful contributions to COVID research,” said Seet, who together with Crooks is studying which parts of the virus might trigger the strongest T-cell response, and thus be most useful in developing an effective vaccine.
The benefits of pivoting to coronavirus science will probably go both ways, he added: “I hope what we learn, we can apply back to immunotherapy.”

(Allen J. Schaben/Los Angeles Times)
Sunny Jiang, a UC Irvine environmental engineer, usually studies wastewater recycling methods and monitors coastal contamination. Now she’s examining the extent to which the coronavirus can be transmitted through aerosols.
The viral outbreak is not just a medical problem, Jiang pointed out. It’s a problem with social, psychological, economic and engineering aspects, among others. So the more researchers who turn their attention to the disease, the better.
“You need diverse minds to look at this problem,” she said. Stopping this pandemic, she said, will require solutions from all walks of science.

