Wall Street Journal: How Barouch’s HIV research laid the foundation for COVID vaccines
Wall Street Journal – December 24, 2020
Dan Barouch, MD, PhD (Center for Virology and Vaccine Research, BIDMC) started a laboratory at BIDMC and Harvard Medical School in 2004 to develop an AIDS vaccine. He noted that if not for developing Ad26 for HIV, they would not already be in phase three trials for a COVID-19 vaccine.
People are receiving Covid-19 vaccines less than a year after public health authorities discovered SARS-CoV-2, the deadly new coronavirus. How did it happen so quickly? In part, the world can thank decades of frustrating and often fruitless research to find a vaccine for Human Immunodeficiency Virus or HIV, the virus that causes AIDS. Many of the new technologies and approaches employed to create potent Covid-19 vaccines and therapies trace their origins to the desperate search, starting in the early 1980s, to slow the spread of HIV.
AIDS has claimed 33 million lives to date, and 38 million people are currently living with HIV. There is still no vaccine. But since 1982, the U.S. has invested more than $76 billion in lifesaving treatments, quietly revolutionizing the development of vaccines and therapies for other viruses, including the coronavirus.
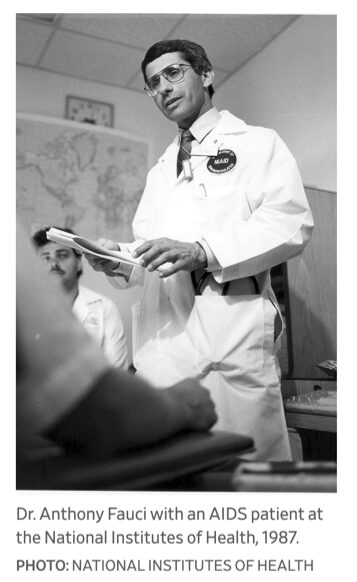
“Everything we do with every other pathogen spins off of things we’ve learned with HIV,” said Anthony Fauci, a leader in HIV research as director of the National Institute of Allergy and Infectious Diseases since 1984.
Scientists haven’t yet been able to develop an effective AIDS vaccine, partly because HIV is one of the most cunning, complex pathogens ever encountered. Like the coronavirus, HIV has a spike or envelope protein that binds to receptors on the surface of cells, but in HIV it doesn’t stay intact long enough to be efficiently attacked by the immune system.
Over decades of work, however, HIV researchers developed a better understanding of the complex workings of the immune system. They mapped out in detail how HIV invades cells and replicates, and identified weak spots in the virus that can be targeted by drugs. Using X-ray crystallography and later electron microscopy, combined with computer modeling, researchers created highly detailed three-dimensional images of proteins on the surface of HIV. The idea was to use the images to engineer antigens, molecules that generate an immune response and prompt the body to mount a defense against the virus.
Scientists such as Barney Graham, deputy director of the NIAID’s Vaccine Research Center, have used a similar approach to design antigens for vaccines against other viruses. In early January, Dr. Graham and his team were preparing to test prototype vaccines for several viruses—including one for Middle East respiratory syndrome, a coronavirus—when they learned about the outbreak of a new coronavirus in China. They quickly shifted gears to the new pathogen, and provided the spike-protein design for the vaccine antigen delivered by the Moderna Inc. vaccine. That vaccine uses messenger RNA, a molecular courier that instructs cells to make the antigen.
“It really was HIV driving most of this, trying to find an HIV vaccine, going through several rounds of failure on that and continuing to improve the technology,” Dr. Graham says.
Even crushing HIV disappointments have paid off in the Covid-19 battle. In 2004, Merck & Co., working with investigators funded by the NIAID, created a vaccine using a weakened common-cold virus called Adenovirus 5. Nicknamed Ad5, this “vector” was used to deliver three genes found in HIV into the body. The hope was that the immune system would attack these foreign genes and learn to fend them off, preparing it for future encounters with actual HIV.
In late 2007, the trial was halted abruptly when early results showed that the vaccine provided little protection and was likely making men more susceptible to HIV. Merck closed its entire AIDS-vaccine effort, but others built on its research, developing vaccines that use different cold viruses, including one affecting chimps, to carry genes from debilitating viruses. This is the approach behind the Covid-19 vaccine recently developed by the University of Oxford and AstraZeneca, which soon could gain approval.
Dan Barouch, who started a laboratory at Boston’s Beth Israel Deaconess Medical Center and Harvard Medical School in 2004 to develop an AIDS vaccine, saw Merck’s setback as proof that he needed to focus on other viral vectors, including one called Ad26, based on an inactivated, rarer human cold virus. Dr. Barouch’s team cloned and developed that vaccine vector in 2007 and went on to work with a small Dutch company and later Johnson & Johnson to develop Ad26 vaccines for Zika and Ebola. The latter is now approved by European regulators.
Those virus epidemics slowed before the team had a chance to fully test their vaccines. But when the new coronavirus emerged this year, Dr. Barouch and J & J went to work on a Covid-19 vaccine that, unlike those produced by Moderna and by Pfizer Inc. and German partner BioNTech SE, has a one-shot protocol and doesn’t need to be stored at subzero temperatures. Interim trial results for that vaccine are expected in January.
“If it weren’t for us developing Ad26 for HIV we wouldn’t already be in phase three for Covid-19,” says Dr. Barouch, who continues to work on an AIDS vaccine. “It’s the direct result of our HIV research, it wouldn’t have been developed otherwise.”
Scientists met frustrations developing drugs to treat HIV, just as they did with vaccines. Eventually, combinations of antiviral pills—including Truvada and Descovy, produced by Gilead Sciences —proved effective, helping to cut death rates by about half over the last decade and prolonging the lives of those with HIV. To produce those drugs, the Foster City, Calif., company developed ways to prevent HIV from replicating by inhibiting the body from copying the virus’s genetic material, a process called “chain termination.” This year, Gilead applied those techniques to the new coronavirus, resulting in its drug remdesivir, which an NIH study found speeds the recovery of hospitalized Covid-19 patients. “We really only began to understand these mechanisms and design compounds to inhibit [replication] while researching HIV,” says Diana Brainard, who heads virology at Gilead.
Other scientists discovered that some HIV patients carried antibodies in their blood that were unusually powerful at neutralizing the virus. Researchers have learned to identify promising antibodies for other viruses and develop therapies out of laboratory versions that mimic the same robust immune response. The U.S. Food and Drug Administration has authorized Covid-19 treatments made with these so-called monoclonal antibodies by Eli Lilly & Co. and Regeneron Pharmaceuticals Inc., whose treatment was given to President Donald Trump when he had Covid-19.
Fittingly, some scientists say that current work on combating Covid-19 may, in turn, finally produce an HIV vaccine. “We’re just going to learn so much about the immunology, about manufacturing, about delivery, about how to dose, how to boost,” says Sharon Lewin, director of the Peter Doherty Institute for Infection and Immunity in Melbourne, Australia. “We will suddenly have a lot of observations and understanding of how these vaccines work in humans. I think it will be an incredible advance.”

